Thumb Arthritis Solutions at Nebraska Hand & Shoulder Institute, P.C.
Living with thumb arthritis can hamper daily activities and lessen your quality of life, especially for women over 40 who are most prone to this condition.
But relief is within reach, thanks to the team of experts at Nebraska Hand & Shoulder Institute, P.C. Specializing in advanced thumb arthritis treatments, including both non-operative and surgical options, they are committed to restoring your hand mobility and alleviating your pain.
Understanding Thumb Arthritis
Thumb arthritis primarily affects the trapeziometacarpal joint (CMC), the joint at the base of your thumb, responsible for its mobility and rotation. This form of arthritis is degenerative and spontaneous, with some rare cases being caused by rheumatoid disease or post-traumatic injuries.
Prolonged untreated thumb arthritis can lead to several complications, including contracture of the first web space and a "swan neck" type of deformity. These conditions can severely affect your ability to grip and pinch, ultimately diminishing your hand's functionality.

X-ray depicting swan neck deformity. Note how the thumb and index metacarpals are pressed tightly together

Contracture of the first web space (the thumb ends up lying closer to the index metacarpal)

Contracture of the first web space & MP joint hyperextended (swan neck deformity)
Identifying Thumb Arthritis Symptoms
People living with CMC arthritis commonly report pain at the base of the thumb or the thumb side of the wrist, particularly during motion and pinching. Other symptoms may include difficulty in gripping objects, frequent dropping of items due to discomfort or loss of dexterity, and visible enlargement over the base of the CMC.
Common symptoms include:
- Pain at the base of the thumb or thumb side of the wrist, especially during movement and pinching
- Difficulty gripping objects
- Frequent dropping of items due to discomfort or loss of dexterity
- Visible enlargement over the base of the CMC

Enlargement at the base of the thumb
Diagnosing Thumb Arthritis
When a person experiences pain at the base of the thumb, the doctor must perform a differential diagnosis to rule out conditions like de Quervain's tendonitis, trigger thumb, and carpal tunnel syndrome. This includes a physical exam with the grind test, which pushes the thumb end toward the wrist and rotates it to cause pain and grating. The doctor checks for localized tenderness, joint range of motion, and grip and pinch strength. X-rays of the wrist confirm and stage arthritis.
Sometimes, a nerve conduction study is recommended to evaluate median nerve entrapment at the carpal tunnel. This is crucial as undetected carpal tunnel issues may require additional surgery. Research shows that over half of those with arthritis at the thumb base also have median nerve entrapment. The cause-and-effect relationship between these conditions remains unclear.
Treatment Goals
- Pain relief
- Strong, functional grip and pinch
- Normal thumb mobility
- Improved appearance
Non-Operative Treatment Options
Once thumb arthritis is diagnosed, initial treatments often include NSAIDs and acetaminophen (Tylenol). If there are no contraindications like ulcers or allergies, a trial of NSAIDs such as meloxicam, Celebrex, naproxen sodium, diclofenac, or topical options like Voltaren gel and ketoprofen cream may be given for at least 3 weeks to assess effectiveness.
If thumb arthritis symptoms persist despite NSAIDs or other initial treatments like cortisone injections and braces, cortisone injections can provide temporary relief but may be painful, while hyaluronic acid injections have limited benefits. Splinting can offer some relief but may hinder daily activities, making surgery a reliable option for enduring relief.
Surgical Treatment
Our skilled team administers several surgical procedures under regional or general anesthesia. Surgery is usually done under regional anesthesia by numbing from the hand to the shoulder or general anesthesia as an outpatient. Surgical treatment of CMC arthritis has evolved over the past 60 years and can be generally categorized into 5 different options:
- Thumb Denervation
- Resection arthroplasty (with or without TightRope suspension)
- Implant arthroplasty (titanium or pyrocarbon)
- Metacarpal osteotomy
- Fusion
Thumb Denervation
For treating arthritis at the base of the thumb, we recommend denervation, a minimally invasive procedure offering the fastest relief with the lowest pain and quickest recovery. While traditional resection (bone removal) procedures are slightly more definitive, they come with significantly more pain and a longer recovery period of about six months.
Denervation is a great initial option as it does not preclude other treatments if needed. It is a definitive procedure with lasting results, though there is a risk of temporary or permanent numbness in a small area around the top of the thumb (never on the palm side). This approach reinforces our commitment to providing effective, patient-centered care.
Depending on the extent of your arthritis, the most suitable treatment will be recommended.
- Resection arthroplasty (with or without TightRope suspension)
- Implant arthroplasty (titanium or pyrocarbon)
- Metacarpal osteotomy
- Fusion

X-Ray Before Tight Rope Suspension Surgery

X-Ray After Tight Rope Suspension Surgery

X-Ray of a Pyrocarbon Implant
WARNING: MAY CONTAIN GRAPHIC IMAGES
Numerous studies show that resection arthroplasty is the best surgical option for thumb arthritis treatment. At Nebraska Hand & Shoulder Institute P.C., we perform this procedure to ensure a pain-free, stable thumb without using foreign materials.
Introduced in 1948, resection arthroplasty often involves using a tendon as a cushion, filling the void left by the removed trapezium bone. For arthritis limited to the trapeziometacarpal joint, titanium or pyrocarbon hemi-arthroplasty may also be viable options.
Arthroscopic Resection
A method for arthroscopic resection of the trapezium was also developed over 20 years ago. Results are comparable to those of the formal open procedure. Using the added technology necessary for arthroscopy does add to operative time and cost, and thus the small gain from the smaller incision has to be carefully weighed as the 3 week recovery time spent wearing a brace has not been reduced.
Treatment of Thumb MP Joint Hyperextension Deformity
For correcting thumb MP joint hyperextension deformity, common in advanced CMC joint arthritis, we use a small incision technique on the palmar aspect of the thumb. This involves tightening the palmar plate or advancing the flexor pollicis brevis muscle, followed by temporary pin placement.
An additional two weeks of immobilization post-surgery ensures proper healing. Dr. Ichtertz reinforces the capsulodesis with a longitudinal scar to maintain alignment, achieving the best results for our patients.

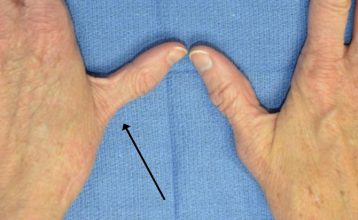
Example of MP joint hyperextension
Fusion of the CMC
This technique is not frequently used. Fusion means to bond one bone to the other so that there is no motion of the joint. Upon fusing the thumb CMC, a person is unable to lay her palm flat, thus it is felt by some to result in an awkward restriction of motion. Additionally, failure of the fusion to unite - especially a problem with smokers - may require additional surgery in order to affect bone union.
During the course of healing over 3 to 4 months, the patient has to wear a brace or cast. Additionally, for a person with arthritis on both sides of the trapezium, which is quite frequent, she would not have the option of fusion because it would entail almost fusing the entire wrist.
Osteotomy
Surgically breaking the metacarpal bone just above the joint has been reported to have good pain relief results in the majority of patients. Exactly how pain is reduced with this technique is uncertain. There is no need for foreign material that might result in a reaction such as silicone or implant loosening.
This procedure is particularly suited for an individual with marked web space contracture wherein the thumb metacarpal is pulled against the index. However, this procedure does not result in improved range of motion because nothing is done directly to the arthritic CMC joint. There is also additional time necessary for bone healing at the osteotomy site, not a necessity when resection arthroplasty or implant arthroplasty are performed.
Total Joint Arthroplasty
Complete replacement of the thumb CMC joint, similar to total knee replacement, is a difficult procedure with disappointing results in most surgeon's hands. In contrast with joint replacement of larger joints such as the hip or knee, there is little bone with which to secure fixation of the implant.
Because of the heavy force the thumb is subjected to, there appears to be a higher rate of loosening. With loosening comes pain and then removal of the implant, i.e. back to the starting point. Thus, total joint replacement of the CMC joint of the thumb is generally not considered a surgical option at this time.
Post-Surgery Care and Rehabilitation
Our care goes beyond surgery to ensure effective thumb rehabilitation. Post-op soreness is common; elevate your hand above the heart for the first week to reduce pain, swelling, and stiffness. Wear a lightweight splint for about 3 weeks, or 6 weeks if a pin is needed for stabilization. Thumb range of motion exercises start between 1 to 3 weeks for patients without a pin. The pin is removed under local anesthesia between 4 and 6 weeks. Strength-building exercises begin at 3 weeks for most patients and at 6 weeks for those with a pin. We support you until you regain full thumb mobility and strength.
Motion is usually recovered within a few days after discontinuing the splint. The main goal, then, is regaining pinch and grip strength. Exercises with TheraPutty, done 3 or more times per day, are crucial; it offers various resistances, with red being intermediate. A spring-loaded toilet paper holder is also great for building pinch strength. Most people experience complete pain relief and improved pinch strength after this surgery.

TheraPutty Exercises

Spring-Loaded Toilet Paper Holder Exercises
Risks of surgery
Any surgery on the base of the thumb includes a risk of temporary numbness, a very small risk of permanent numbness, or hypersensitivity from injury to superficial nerves. There is about a 1 in 200 chance of infection. Blood loss is minimal. Only implant arthroplasty is associated with dislocation and possible foreign body reaction, such as silicone synovitis.
A small change in measurable pinch strength occurs but is outweighed by elimination of pain. However, patients rarely perceive weakness once fully healed. Occasionally the base of the thumb ends up being mildly enlarged or puffy. This probably relates to scar and subtle settling of the thumb and can't be helped. It does not affect pain relief or function.
Results of Resection Arthroplasty
As noted below, marked relief of pain and restoration of function and motion are achieved in the majority of patients treated with CMC arthroplasty.
- P. Amadio, M.D. in 1982 reported 94% satisfaction
- R. Burton, M.D. in 1986 reported 92% satisfaction
- J. Menson, M.D. in 1981 reported 96% satisfaction
- A. Swanson, M.D. in 1997 reported 97% satisfaction
Which Do You Prefer?

This patient has had surgery on the right thumb. Notice how the left thumb is still deformed?
Trust Nebraska Hand & Shoulder Institute, P.C. for your Thumb Arthritis Treatment
Nebraska Hand & Shoulder Institute, P.C. is your trusted partner in managing thumb arthritis. With a team of experienced physicians and state-of-the-art facilities, we are here to help you rediscover a life free from arthritis pain. Reach out to us today to schedule an appointment.
Amadio P, Millender L, Smith R: Silicone spacer or tendon spacer for trapezium resection arthroplasty -comparison of results. J Hand Surg 1982; 7:237.
Calandruccio J, Jobe R: Arthroplasty of the thumb carpometacarpal joint. Seminars in Arthroplasty 1997: 135-147.
Badger E: Arthrodesis of the carpometacarpal joint of the thumb. J Bone Joint Surg 1964; 46B:16.
Bunnell S: Surgery of the Hand: 3rd Edition, Philadelphia J.B. Lippincott Co. 1956; 823.
Bossley CJ: Basal osteotomy of the first metacarpal for osteoarthritis of the first carpal metacarpal joint. J Bone Joint Surg 1981; 63B:468.
Brase DW, Millander LH: Failure of silicone rubber wrist arthroplasty in rheumatoid arthritis. J Hand Surg 1986; 1A:175.
Burton R, Pellegrini VD: Surgical management of basal joint arthritis of the thumb Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg 1986; 11A:324.
Carroll RE, Hill NA: Arthrodesis of the carpometacarpal joint of the thumb. J Bone Surg 1973; 55B:292.
Carter PR, Benton LJ, Dysert PA: Silicone rubber carpal implants: a study of the incidence of late osseous complications. J Hand Surg 1986; 11A:639.
Dell PC, Brushart TM, Smith RJ: Treatment of trapeziometacarpal arthritis: results of resection arthroplasty. J Hand Surg 1978; 3:243.
Eaton RG: Replacement of the trapezium for arthritis of the basal articulations. A new technique with stabilization of tenodesis. J Bone Joint Surg 1979; 61A:76.
Eaton RG, Glickel SZ, Littler JW: Tendon interposition arthroplasty for degenerative arthritis of the trapeziometacarpal joint of the thumb. J Hand Surg 1985; 10A:645.
Eaton RG, Littler JW: A study of the basal joint of the thumb: treatment of its disabilities by fusion. J Bone Joint Surg 1969; 51A:661.
Eiken O, Carstam N: Functional assessment of basal joint fusion of the thumb. Scand J Plast Rec Surg 1983; 53:219.
Florack T et al: The prevalence of carpal tunnel syndrome in patients with basal joint arthritis of the thumb. J Hand Surg 1992; 17A:624-630.
Gervis WH: Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint. J Bone Joint Surg 1949: 31B:540.
Gervis WH: A review of excision of the trapezium for osteoarthritis of the trapeziometacarpal joint after twenty-five years. J Bone Joint Surg 1973; 55B:56.
Gordon ML, Bullough PG: Synovial and osseous inflammation in failed silicone rubber prostheses. J Bone Joint Surg 1982; 64A:574.
Graber-Duvernay JB, Graber-Duvernay JL: Remarques sur la rhizarthrose du pouce (d’apres 500 observations). Rev Lyon Med 1970; 19:209.
Haffajee D: Endoprosthetic replacement of the trapezium for arthrosis of the carpometacarpal joint of the thumb. J Hand Surg 1977; 2:141-148.
Haraldsson S: Extirpation of the trapezium for osteoarthritis of the first carpometacarpal joint of the thumb. Acta Orthop Scand 1972; 43:347.
Iyer KM: The results of excision of the trapezium: 26 cases of excisional arthroplasty. Hand 1981; 3:246.
Menon J, Schoene HR, Hohl JC: Trapeziometacarpal arthritis. Results of tendon interpositional arthroplasty. J Hand Surg 1981; 6:442-446.
Murley AH: Excision of the trapezium in osteoarthritis of the first carpal metacarpal joint. J Bone Joint Surg 1960; 42B:502.
Pallegrini V, Burton R: Surgical management of basal joint arthritis of the thumb. Part 1: Long-term results of silicone implant arthroplasty. J Hand Surg 1986; 11A.
Swanson A: Trapezium implant arthroplasty. J Hand Surg 1981; 6A:125-141.
Swanson A, Swanson G, DeHeer D, Pierce T, Randall K, Smith J, VanGorp C: Carpal bone titanium implant arthroplasty. Clinical Ortho 1997; 342:46-58.
Thompson TC: Surgical treatment of trapeziometacarpal arthrosis. Advances in Ortho Surg 1986; 105-120.
Varley GW, et al: Excision of the trapezium for osteoarthritis at the base of the thumb. J Bone Joint Surg ;76B,6; 964-968.
Weilby A, Sondorf J: Results following removal of silicone trapezium metacarpal implants. J Hand Surg 1978; 3:154.
Wilson JN: Basal osteotomy of the first metacarpal in the treatment of arthritis of the carpometacarpal of the thumb. British J Surg 1973; 60:854-58.
Wilson JN, Bossley CJ: Osteotomy in the treatment of osteoarthritis of the first carpal metacarpal joint. J Bone Joint Surg 1983; 65B, 2:179-181.