Ulnar Wrist Pain
Do you have persistent pain along the outer edge of your wrist? This may be ulnar wrist pain, a condition also known as pain on the pinky side of the hand or ulnar-sided wrist pain. These symptoms often indicate nerve compression or structural injury and require an accurate diagnosis for long-lasting relief.
At the Nebraska Hand & Shoulder Institute, our board-certified orthopedic surgeon Dr. Ichtertz and his expert team specialize in diagnosing and providing ulnar wrist pain treatment. Whether you're dealing with mild discomfort or chronic ulnar wrist pain, we create treatment plans tailored to your specific condition.
Finding the exact cause of your wrist discomfort is the first step toward recovery. With years of experience treating complex hand and wrist problems, we offer a full spectrum of wrist pain treatment options to help restore your comfort and function.
If you’re living with outside wrist pain, don’t wait. We proudly serve Omaha, Lincoln, and Grand Island. Contact us today to begin your personalized treatment plan.
Understanding Ulnar Wrist Pain
The ulna is the smaller of the two forearm bones and runs along the same side as the pinky finger. When pain develops on this side of the wrist, it’s called ulnar-sided wrist pain or pain on the pinky side of the hand. This condition often affects adults, especially men in their late twenties to forties. It usually follows an injury such as a fall on an outstretched hand, with or without a wrist fracture.
Effective ulnar wrist pain treatment starts with a detailed history and physical exam. With the right evaluation, most cases improve significantly or resolve entirely. Over the past decade, advancements in arthroscopic surgery and diagnostic tools have greatly enhanced wrist pain treatment outcomes.
If left untreated, chronic ulnar wrist pain may reduce grip strength, interrupt sleep, and interfere with daily activities. It can also lead to long-term functional decline and decreased productivity.
Anatomy
The wrist, or carpus, is a complex joint made of eight small bones, along with the ends of the radius and ulna. These bones move in four directions: upward (dorsal), downward (palmar), and side-to-side (radial and ulnar). These motions are essential for grip, precision, and overall hand function.
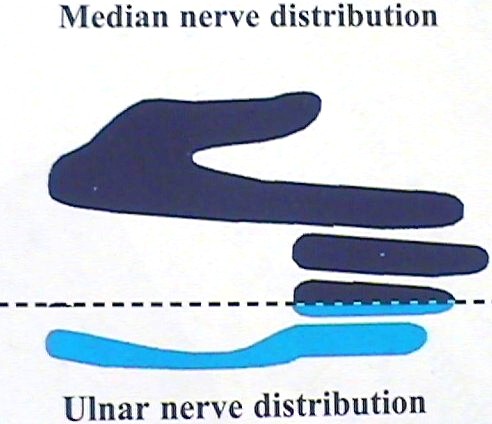
The ulnar side of the wrist, where most ulnar wrist pain occurs, is innervated by the ulnar nerve. This nerve can become compressed at either the wrist or the elbow, leading to symptoms such as outside wrist pain, numbness, burning, or aching. Patients often report difficulty writing, gripping, or completing repetitive tasks, especially if the condition becomes chronic.
Understanding this nerve distribution is key to delivering accurate ulnar wrist pain treatment, particularly for individuals experiencing persistent discomfort on the pinky side of the hand.
Differential Diagnoses & Causes
1) Ulnar Tunnel Syndrome
Ulnar Tunnel Syndrome causes numbness, burning, clumsiness, and ulnar sided wrist pain, especially on the pinky side of the hand. These symptoms often occur alongside signs of carpal tunnel syndrome, which is why it’s important to evaluate both the cubital tunnel and Guyon’s canal for ulnar nerve compression.
Guyon’s canal, or the ulnar tunnel, sits next to the carpal tunnel, separated by a septum. When a carpal tunnel release is performed, the procedure often decompresses the ulnar nerve at the same time. This explains why many patients experience relief from outside wrist pain and hand numbness without needing additional surgery on the ulnar tunnel.
An easy comparison: decompressing the carpal tunnel is like removing extra passengers from a crowded bench seat. With the pressure gone, the remaining nerves have more space and improved function.
Imaging studies using CT and MRI show that carpal tunnel release can increase the tunnel’s volume by about 25%, reducing pressure. Isolated ulnar tunnel decompression is rarely needed, but when it is, we investigate potential causes like ganglion cysts within the canal.
While Richman and Gelberman (1989) suggested Guyon’s canal changes shape after decompression, our clinical experience indicates the benefit is more related to the redistribution of space than to structural transformation.
Pressure on the ulnar nerve causing the muscle to spasm.

No pressure on the ulnar nerve.
2) Cubital Tunnel Syndrome
Cubital Tunnel Syndrome results from compression of the ulnar nerve at the elbow. It typically affects people over the age of 30 and is seen about three times more often in women than in men. One of the most common causes is sleeping with the elbow bent, which places prolonged pressure on the nerve.
While this condition often causes tingling or numbness in the fingers, it can also lead to ulnar wrist pain or radiating outside wrist pain along the arm. Recognizing these symptoms early allows for more effective ulnar wrist pain treatment and may prevent long-term discomfort or functional limitations.

Improper Sleep Posture
3) Torn Triangular Fibrocartilage (TFCC)
A torn Triangular Fibrocartilage Complex (TFCC) is a common cause of ulnar wrist pain, especially in active individuals or those who have experienced wrist trauma. Patients usually report tenderness on the top of the wrist. Pain often worsens with ulnar deviation (moving the hand toward the pinky side), gripping, twisting, or impact activities like pounding.
This type of ulnar sided wrist pain is most reliably diagnosed with an arthrogram or wrist arthroscopy, which allows for direct visualization of the injury. While MRI can detect TFCC tears, it is typically more expensive and less consistent. Swelling in the area may indicate synovitis—an inflammatory response due to joint or tendon lining engorgement.
Without treatment, a torn TFCC can lead to chronic ulnar wrist pain and reduced function. A timely and accurate diagnosis is key to developing an effective ulnar wrist pain treatment plan based on the severity of the tear and the patient’s lifestyle demands.
Outcome of Surgery for Torn TFCC
| Procedure | Surgeon | Outcome |
| Arthroscopic Trimming | Melone 1991 | 83% Good/Excellent |
| Osterman 1990 | 88% Good/Excellent | |
| Ulnar Shortening | Melone 1998 | 92% Good/Excellent |
| Hulsizer 1997 | 91% Excellent |

Example of normal TFCC

Example of torn TFCC
4) Kienbock’s Disease
Kienbock’s Disease is a rare condition that involves the loss of blood supply (bone infarct) to the lunate bone in the wrist. This leads to bone deterioration over time and can cause ulnar wrist pain, especially if the lunate collapses and puts pressure on nearby structures on the ulnar side of the wrist. The exact cause of Kienbock’s remains unknown.
Treatment depends on how far the disease has progressed. In early stages, the goal is to relieve pressure on the lunate and restore blood flow, often using a vascularized bone graft or artery. If the bone has already broken down, salvage procedures like wrist fusion or Proximal Row Carpectomy (PRC) may be necessary.
Although several wrist pain treatment strategies are available for Kienbock’s Disease, patient satisfaction rates hover around 70%, which suggests that outcomes vary and treatment should be highly individualized.

Bone appears more solid due to loss of blood flow causing it to die and crumble.
5) Ulnocarpal Abutment
Ulnocarpal abutment, also known as ulnar impaction syndrome, is a mechanical cause of ulnar wrist pain. It happens when the ulna presses abnormally against the small wrist bones, often damaging the Triangular Fibrocartilage Complex (TFCC). This ongoing pressure can result in chronic ulnar wrist pain and soft tissue degeneration over time.
The condition frequently develops after a wrist fracture heals unevenly, leaving the ulna longer than it was before the injury. Degenerative growth disturbances can also contribute. As a result, excess pressure builds up on the ulnar side of the wrist, which may crush or tear the TFCC.
Accurate diagnosis is key to selecting the right ulnar wrist pain treatment. One of the most effective options is surgical shortening of the ulna, which restores joint balance and reduces painful contact between the bones.
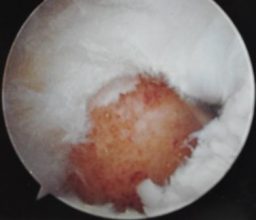
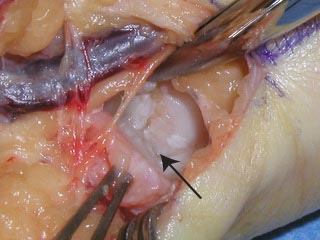
End of trimmed ulna as seen through hole in TFCC


6) Ulnar Artery Thrombosis (Hypothenar Hammer Syndrome)
Ulnar artery thrombosis, also called Hypothenar Hammer Syndrome, is a rare vascular condition that may contribute to ulnar wrist pain and circulation problems in the fingers. It typically affects individuals over age 50, especially heavy smokers who frequently perform high-impact hand activities like hammering, pounding, or tool use.
This condition occurs when repeated trauma causes clotting in the ulnar artery, which reduces blood flow to the hand. Patients often develop fingertip lesions, numbness, or discoloration.
Effective ulnar wrist pain treatment in these cases involves correcting the underlying vascular issue. Lifestyle adjustments and changes to repetitive hand movements are also important in managing symptoms and preventing recurrence.

Finger tip ulcer at different stages of healing after circulation cut off by tiny clots

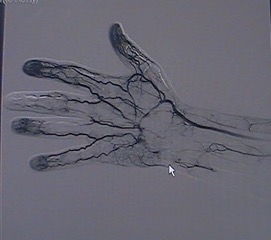
Arthrogram showing blocked ulnar artery
7) Ganglion Cyst
A ganglion cyst is a fluid-filled sac that develops from a joint or tendon sheath. These cysts commonly appear on the wrist and are typically benign. While many are painless, some ganglion cysts press on nearby nerves or tissues, causing ulnar wrist pain or localized discomfort.
If a ganglion contributes to outside wrist pain or starts to interfere with hand function, surgical removal may offer the most effective ulnar wrist pain treatment. Although results are usually successful, about 15% of cysts can recur.
Evaluating whether a ganglion cyst is the source of wrist discomfort is essential, especially when symptoms overlap with other wrist conditions.

8) Piso-Triquetral Arthritis
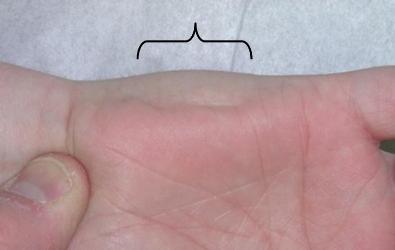
Piso-triquetral arthritis is an uncommon form of joint degeneration that affects the small joint between the pisiform and triquetrum bones on the ulnar side of the wrist. The pisiform is a vestigial bone that serves little functional purpose, making it a common target for surgical removal when ulnar wrist pain becomes persistent.
This condition typically causes pain on the pinky side of the hand, especially during activities that put pressure on the heel of the hand. In cases involving broader joint issues, NSAIDs may help reduce inflammation. However, if symptoms continue, removing the pisiform offers an effective and low-risk ulnar wrist pain treatment. Most patients experience full pain relief and a fast recovery after the procedure.

9) Extensor Carpi Ulnaris Tendinosis
Extensor Carpi Ulnaris (ECU) tendinosis is a condition that causes inflammation in the ECU tendon, which helps lift the wrist and move it toward the pinky side. This muscle plays a vital role in wrist stability and function. Although the exact cause remains unclear, ECU tendinosis is comparable to de Quervain’s tendinosis, which affects the thumb side of the wrist.
In recent years, this condition has become a more common source of outside wrist pain and ulnar sided wrist pain. Patients often experience symptoms that worsen with repetitive motion or lifting activities. For many, it becomes a form of chronic ulnar wrist pain.
The first line of ulnar wrist pain treatment typically includes a cortisone injection to reduce inflammation. If pain persists, a minor outpatient procedure through a small incision on the back of the wrist can provide fast relief. No cast is needed after surgery, and scarring is minimal.
Some patients may experience temporary numbness around the incision site due to the nearby dorsal cutaneous branch of the ulnar nerve, which is carefully protected during the operation. This condition appears equally in people who do manual labor and those with desk jobs.
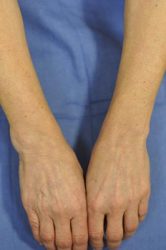
Note the swelling in the exterior of the wrist on the left
10) Carpal Instability (Lunotriquetral Instability)
The wrist joint includes eight small bones that connect with the radius and ulna in the forearm and the metacarpals in the hand. On the pinky side of the wrist, instability can occur between the lunate and triquetrum bones. This rare condition, called lunotriquetral instability, is a known cause of ulnar sided wrist pain and often results from trauma, such as a fall onto an outstretched hand.
When tendons and ligaments between these small wrist bones are damaged, the joint becomes unstable. This can lead to ongoing pain, reduced grip strength, and loss of function, especially if left untreated. Over time, it may develop into chronic ulnar wrist pain.
To confirm the diagnosis, our specialists use X-rays, MRI scans, or wrist arthroscopy. Once diagnosed, the most effective ulnar wrist pain treatment is lunotriquetral fusion, a procedure that stabilizes the bones and relieves pain caused by abnormal joint movement.


Advanced Ulnar Wrist Pain Treatment in Nebraska
At the Nebraska Hand & Shoulder Institute, we offer specialized ulnar wrist pain treatment for patients facing injury, nerve issues, or degeneration. Our experienced team provides personalized care tailored to your diagnosis, whether you're recovering from trauma or managing chronic ulnar wrist pain. We proudly serve communities in Omaha, Lincoln, and Grand Island.
Our treatment process starts with a hands-on examination and in-depth review of your symptoms. We identify the exact source of discomfort and use advanced imaging, such as X-rays and MRI scans, to rule out conditions like avascular necrosis. If a ligament tear is suspected, we may recommend an arthrogram (a contrast dye injection) or wrist arthroscopy for clearer insight.
Depending on your diagnosis, we customize your wrist pain treatment plan. In many cases, pain stems from damage to the Triangular Fibrocartilage Complex (TFCC). When this occurs, Dr. Ichtertz may perform a minimally invasive outpatient procedure to trim the TFCC using a fiberoptic scope inserted through small punctures in the wrist.
If you have ulnocarpal abutment, we may recommend shortening the ulna. This surgical technique removes a small bone wedge and stabilizes the area with a plate and screws. Thanks to secure fixation, most patients heal in 8 to 12 weeks without needing a cast.
In cases involving joint degeneration or instability, we may suggest limited carpal fusion or a Proximal Row Carpectomy (PRC). These options help relieve pain while preserving wrist movement.
Dr. Ichtertz has over a decade of experience performing advanced procedures for pain on the pinky side of the hand. If you're struggling with outside wrist pain or persistent discomfort, trust our team for proven solutions and lasting relief.

Proximal Row Pre-Op

Proximal Row Post-Op
Risks of Wrist Surgery
Many wrist procedures offered for ulnar wrist pain treatment are minimally invasive and done on an outpatient basis. These surgeries typically involve low discomfort after the procedure. Still, every surgery carries some risk.
Possible complications include infection, nerve irritation, or increased wrist pain. In surgeries like wrist fusion, there is a small chance of non-union, where the bones do not heal properly. This risk is slightly higher in patients who smoke and may require a second procedure to resolve. Some individuals may also develop noticeable scarring, particularly those with darker skin tones.
We explain these risks clearly before surgery so you can make an informed decision. Our team prioritizes your safety and works to reduce complications while providing effective wrist pain treatment.
Schedule Your Wrist Pain Appointment Today
Ulnar wrist pain is not only difficult to diagnose but also challenging to manage. You don't have to deal with it on your own. At Nebraska Hand & Shoulder Institute, Dr. Ichtertz and his skilled team focus on identifying the root cause of your discomfort. Whether you're dealing with chronic ulnar wrist pain or outside wrist pain that interferes with your daily routine, we provide precise, effective treatment.
We begin with conservative care whenever possible. Our ulnar wrist pain treatment approach often includes anti-inflammatory medication, splinting, and targeted injections. While physical therapy is not our standard recommendation for most wrist and hand conditions, we prioritize treatments that reduce pain quickly and restore hand function without unnecessary delays.
Our goal is to help you stay active and productive. Each treatment plan is customized to relieve pain on the pinky side of the hand while preserving motion and strength.
Don’t let wrist discomfort keep you from enjoying life. Schedule your appointment with the Nebraska Hand & Shoulder Institute today and take your first step toward long-term wrist pain relief.
Allan CH, Joshi A, Lichtman DM: Kienböck’s disease: diagnosis and treatment. Am Academy Ortho Surg 2001; 9:128-136.
Bain GI, Pugh MW, MacDermid JC, Roth JH: Matched hemiresection interposition arthroplasty of the distal radioulnar joint. J Hand Surg 1995; 20A:944-950.
Begley BW, Engber WD: Proximal row carpectomy in advanced Kienböck’s disease.
Chidgey LK: The distal radioulnar joint: problems and solutions. J Am Acad Ortho Surg 1995; 3:95-109.
Constantine KJ, Tomaino MM, Herndon JH, Sotereanos DG: Comparison of ulnar shortening osteotomy and the wafer resection procedure as treatment for ulnar impaction syndrome. J Hand Surg 2000; 25A:55-60.
DiBenedetto MR, Lubbers LM, Coleman CR: Long-term results of the minimal resection Darrach procedure. J Hand Surg 1991; 16A:445-450.
Hulsizer D, Weiss A-PC, Akelman E: Ulna-shortening osteotomy after failed arthroscopic debridement of the triangular fibrocartilage complex. J Hand Surg 1997; 22A:694-698.
Kirschenbaum D, Coyle MP, Leddy JP: Chronic lunotriquetral instability: diagnosis and treatment. J Hand Surg 1993; 18A:1107-1112.
Minami A, Kato H: Ulnar shortening for triangular fibrocartilage complex tears associated with ulnar positive variance. J Hand Surg 1998; 23A:904-908.
Osterman AL: Arthroscopic debridement of triangular fibrocartilage complex tears. J Arthro Related Surg 1990; 6(2):120-124.
Palmer AK: Triangular fibrocartilage disorders: injury patterns and treatment. J Arthro Related Surg 1990; 6(2):125-132.
Palmer AK, Werner FW, Glisson RR, Murphy DJ: Partial excision of the triangular fibrocartilage complex. J Hand Surg 1988; 13A;403-406.
Palmer AK, Werner FW: The triangular fibrocartilage complex of the wrist - anatomy and function. J Hand Surg 1981; 6(2):153-162.
Pin PG, Young VL, Gilula LA, Weeks PM: Management of chronic lunotriquetral ligament tears. J Hand Surg 1998; 14A:77-83.
Richman JA, Gelberman RH, Rydevik BL et al. Carpal tunnel syndrome: morphologic changes after release of transverse carpal ligament. J Hand Surg 1989; 14A:852-857.
Shin AY, Sheetz KK, Bishop AT, Berger RA: Vascularized pedicled bone grafts from the distal radius: technique and results of treatment for scaphoid nonunion and Kienböck’s disease. Mayo Clinic 1997.
Simmons SP, Tobias B, Lichtman DM: Lunate revascularization with artery implantation and bone grafting. J Hand Surg 2009; 34A:155-160.
Tomaino MM: The importance of the pronated grip x-ray view in evaluating ulnar variance. J Hand Surg 2000; 25A:352-357.
Watanabe T, Takahara M, Tsuchida H, Yamahara S, Kikuchi N, Ogino T: Long-term follow-up of radial shortening osteotomy for Kienböck’s disease. JBJS Am 2008; 90:1705-1711.